Catherine Marshall, MD, MPH, an assistant professor of oncology at Johns Hopkins Medical Center in an interview with GU Oncology helped clarify current changes in the therapy of metastatic hormone sensitive prostate cancer (mHSPC). When we talk about mHSPC, we really mean two things, according to Dr. Marshall: (1) confirmed metastatic disease based on conventional scans (eg, CT or nuclear bone scans) showing evidence of lymphadenopathy (involved lymph nodes), visceral disease (metastases to soft-tissue sites other than lymph nodes), or bone lesions on bone scan; and (2) recently diagnosed prostate adenocarcinoma that has not yet been treated with hormone therapy (ADT).
Dr. Marshall stated that the development and expanded usage of imaging, such as prostate-specific membrane antigen (PSMA) positron emission tomography (PET) are expected to increase the upstaging of prostate cancer in patients. Indeed, in a patient with rising PSA and negative conventional scans (ie, CT and bone imaging), upstaging of a disease that was earlier regarded as biochemically recurrent (Increases in PSA only) may have PSMA imaging diagnostic of metastatic cancer.
ADT has long been the gold standard of care for males with mHSPC, with either a luteinizing hormone-releasing hormone (LHRH) agonist or antagonist being used alone. Unfortunately, men with mHSPC who are treated with ADT alone are almost guaranteed to acquire hormone-resistant illness (prostate cancer that does not respond to ADT). Various antiandrogen therapies have been added to the regimen over the last decade to prevent the inevitable establishment of hormone resistance.
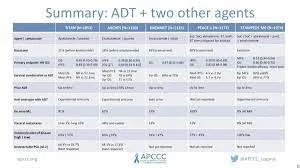
Currently, four medications that were previously only approved for the treatment of hormone-resistant prostate cancer have become the standard of care for men with mHSPC. Docetaxel (Taxotere) and the oral antiandrogens abiraterone, enzalutamide, and apalutamide have been shown in large trials to prolong overall survival when used at the time of diagnosis (i.e., when the patient is still sensitive to ADT) rather than waiting for the disease to progress to metastatic hormone-resistant prostate cancer. Dr. Marshall defined "doublet therapy" as a regimen of ADT plus one of these four approved therapeutic medicines for the treatment of men with mHSPC.
Triplet vs. Doublet Therapy
Since doublet therapy provides a clinical benefit, the obvious next question is whether "triplet therapy" provides an even bigger benefit. Dr. Marshall was careful to moderate expectations when asked this question. She referenced the PEACE-1 trial and the ARASENS trial as two recent randomized trials looking into the benefits of triplet therapy. The main question with triplet therapy, according to Dr. Marshall, is whether "combining chemotherapy with an oral new hormonal drug enhances outcomes relative to chemotherapy and ADT." PEACE-1 investigated the addition of abiraterone/prednisone, whilst ARASENS investigated the addition of darolutamide to the backbone of ADT plus docetaxel.
Dr. Marshall did, however, notice certain disparities in the patient groups of these trials. PEACE-1 patients had de novo metastatic illness (i.e. disease that was metastatic at the time of the prostate cancer diagnosis). Men who had abiraterone with or without radiation in addition to ADT with docetaxel had better radiologic progression-free survival and overall survival, according to the findings. The ARASENS trial, on the other hand, compared ADT plus docetaxel to either the antiandrogen darolutamide or placebo. The majority of patients, but not all, had metastatic disease at the time of diagnosis. ARASENS also demonstrated that triplet therapy outperformed ADT plus docetaxel in terms of overall survival, with the probability of death in the darolutamide group being 32% lower than in the placebo group. Neither of these trials compared ADT and docetaxel plus an oral antiandrogen to a comparator arm of ADT plus an oral antiandrogen alone. As a result, according to Dr. Marshall, we cannot claim with certainty that triplet therapy is superior to doublet therapy with ADT + oral anti-androgen.
One of the primary concerns about the use of triplet therapy, according to Dr. Marshall, is the danger of toxicity to the patient. Concerns have been raised in the medical community concerning the possibility of additive toxicity while taking three medications at the same time. The most serious of these is concern about the possibility of docetaxel exacerbating tiredness and neuropathy. However, those trials revealed "toxicities that would be predicted from the particular drugs," according to Dr. Marshall.
As previously stated, the four standard-of-care medicines used alongside ADT were previously solely advised for hormone-resistant prostate cancer. Dr. Marshall stressed that deciding on the appropriate sequencing of treatments will continue to be increasingly difficult as more treatments become available in clinical practice and the standard treatments for hormone-resistant disease continue to be used earlier in the prostate cancer course. Furthermore, as the medical community continues to use novel hormonal drugs and chemotherapy in the hormone-sensitive situation, the decision about which treatments to use next—after hormone resistance develops—has grown hazy.
Dr. Marshall described the CARD trial as a study that gives data to justify the use of the chemotherapeutic drug cabazitaxel when disease progression has occurred on abiraterone or enzalutamide with docetaxel. The CARD study results indicated a significant improvement in both progression-free survival and overall survival. Dr. Marshall was also careful to point out that the medical community will be required to consider when to use newer therapeutic agents, such as radiologic-targeted lutetium-177 PSMA therapy, immunotherapy, and targeted agents, such as PARP (poly adenosine diphosphate-ribose polymerase) inhibitors, for the treatment of men who may benefit from those therapies.
The Future of mHSPC Treatment GU Oncology also asked Dr. Marshall what the future of mHSPC treatment would look like. She believes that the future of illness management will include the use of more focused medications at earlier stages of the disease. She believes that as medication research and clinical trial progress, the medical community will become better at determining who needs the most rigorous treatment and who can be treated effectively without the additional morbidity that comes with treatment intensification.
Finally, Dr. Marshall emphasized that treatment for males with mHSPC must be adjusted to a variety of patient- and disease-specific characteristics. The current standard of care for males with mHSPC has advanced much beyond the old norm of ADT alone. The paradigm has altered as the use of chemotherapy or novel antiandrogen medicines in combination with ADT has shown considerable survival improvements over ADT alone. Although some people may not benefit from doublet therapy because they are too fragile to tolerate the second agent or have other substantial comorbidities, it is evident that for many patients, there are significantly more treatment alternatives to consider when deciding how to approach a patient with mHSPC.
The original conversation was published online at: https://dialysisinc.com/news/editors-talk-triplet-versus-doublet-therapy-in-metastatic-hormone-sensitive-prostate-cancer/